Personal Update
First of all, happy New Year everyone! At the turn of another year, it feels like a good time to finally let loose the little secret I’ve been keeping and tell you why I’ve been a bit distracted from my writing.
I’m pregnant! Nearly 22 weeks, in fact. My husband and I are obviously overjoyed, but I want to share the story of how it’s been so far. Pregnancy is hard. It’s hard for everyone—don’t let anyone tell you otherwise. The pregnancy ‘glow’ is a total myth, and I’m convinced that those who do seem to be glowing in health are probably suffering just as much as the next tired mother-to-be.
But for some of us, it’s tougher still.
It’s been a rough road to get here, and so I’ve had plenty of days where I was too tired, cranky or exhausted to write. First of all, it’s an IVF pregnancy. If you don’t know what IVF (in-vitro fertilization) is, just know it’s fertility treatment, and involves a heck of a lot of needles and medications which all have to be perfectly timed over the course of 1-2 months, with a gazillion ultrasounds and medical procedures. I went through this twice—once from March to April and then again from July to August. In early September, my husband and I finally received the great news that it had worked!
Then, just after 8 short weeks, I started bleeding—every pregnant woman’s worst nightmare. In my case, the bleeding was due to a subchorionic hematoma, a pocket of blood that had formed between the wall of my uterus and baby’s gestational sac. Though it’s not often talked about, this is actually a very common condition. But usually the bleed is small, and they disappear within a couple of weeks. Large ones pose more of a concern—if the hematoma works its way around to the placenta, it can disrupt the placenta and cause it to either partially or completely detach. This can be catastrophic, so they like to keep a close eye on them.
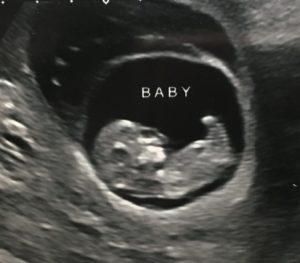
Baby at 11.1 weeks – the large bubble above baby is the subchorionic hematoma
I had fortnightly ultrasounds after this was discovered, to check it was going away. Over the next three ultrasounds, the hematoma continued to grow, and I was getting frequent bleeding and abdominal cramps, so with the support of my doctors I made the decision to stop work completely and I rested at home. The cramps soon went away with more rest, but I had bleeding almost every day for two months before it finally started to stabilize, and eventually the bleeding stopped.
By then, it was time for my anatomic ultrasound. I was feeling optimistic: I hadn’t had any bleeding for two entire weeks, and was beginning to feel some movement which gave me a lot of reassurance that baby was developing well despite all the drama.
What we received was a mixed bag of news: Baby was looking healthy and happy, and we found out baby is a girl! She has a small choroid plexus cyst in the brain (which sounds absolutely terrifying, I know) but these cysts can often happen in normal developing babies and don’t affect the brain’s development, so the radiologist wasn’t worried about her health. What was more concerning, is that I have been diagnosed with placenta previa, vasa previa, and velamentous cord insertion. Phew I know, what a combo.
You probably didn’t expect to have an anatomy lesson on placental conditions in pregnancy, but I’m going to go ahead and explain it all because there is a real lack of awareness out there about these conditions, even within the medical community which is honestly a bit terrifying. So bear with me.
Lots of people have heard of placenta previa, a condition where the placenta overlies the cervical os (baby’s exit point). Because the placenta is what supplies baby with oxygen and nutrients, they can’t let you have birth naturally, as it could cause severe hemorrhage, and the placenta could detach before baby’s safely delivered. Women with placenta previa are more likely to experience bleeding as the placenta is not as firmly attached as it would be higher up in the uterus. But it’s not all bad—the placenta can often move as the uterus grows, and up to 90% of people with placenta previa have the condition resolve before the baby’s birth.
Vasa previa is a whole different kettle of fish. Many people get vasa previa and placenta previa confused, as they sound very similar. Vasa previa is a very rare condition where the blood vessels from baby’s cord lie across or close to the cervical os. Though both conditions are dangerous, vasa previa is arguably more-so (at least for baby) because if these vessels burst then baby can bleed out and die within a matter of minutes. Whereas in placenta previa, there’s usually a bit more time to act before baby is in danger, as it’s the mother’s blood and not the baby’s (baby has less than 300ml when they’re born, so a lot less than an adult!). Velamentous cord insertion refers to the way the cord inserts into the placenta, and often (but not always) this condition goes hand in hand with vasa previa, because the condition makes it more likely the vessels will be close to the cervix. Instead of the cord inserting in the middle of the placenta, the cord runs flat along the uterus and inserts at the edge of the placenta. The vessels are more vulnerable than usual, as at the point of insertion they aren’t tightly bound in a cord.
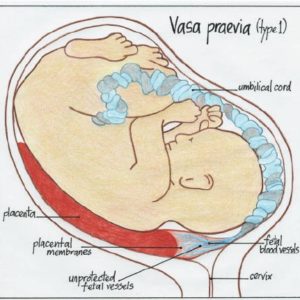
The vessels can move away from the cervix with growth of the uterus, but it’s a lot less likely. And, like with placenta previa, you can’t have a natural birth with vasa previa. If allowed to have a natural birth, most babies will die when the blood vessels rupture from the pressure of labor. The lucky babies who survive often need blood transfusions and resuscitative measures. So, instead they usually do a caesarean section at 34-36 weeks’ gestation which, thankfully, increases survival rates to 97%.
I count myself fortunate to live in a place where the healthcare system is first-rate. In other places and countries, I might not have been so lucky—many women go undiagnosed. The fact that they use color doppler ultrasound (the only way to detect the blood vessels) at every clinic in my city means it was caught very early. Now it’s just a waiting game with many more ultrasounds ahead of me to keep a close eye on my condition.
So, that’s what’s been going on for me over the last few months. It’s been a ride so far, but even with all of this going on in the background, I wouldn’t change it for the world. I’m keeping on, looking for the light at the end of the tunnel, and trusting that the universe has a plan.











Thanks for sharing, it’s great to raise awareness of these things. It’s crazy the new level of stress and worry that being a mum-to-be can bring! I wish you a peaceful rest of your pregnancy.
Thank you!
Congratulations! I have done IVF. Actually, because I’m older, I used a donated embryo, and the procedure is called FET (Frozen Embryo Transfer). I’ve only done one cycle. No baby that time, but I’m hoping next time will be successful. I hope all goes well, and it sounds like they are taking excellent care of you. Sending you all my love as you go through this.
Thank you for the good wishes. Sorry to hear you have to go through fertility treatment too, it’s not easy. But, it is amazing how many women have fertility treatment—being open about it has really highlighted that for me. Someone said I was brave to share it but sharing has honestly opened up so many friendships! We have two embryos left from our last round (unfortunately none from the first, that round was a total flop) and will be doing FET in the future to hopefully have a sibling for this wee girl. Sending my love and good vibes to you for your next round of FET! Donor embryos is a beautiful way to grow your family